From the bedroom – the Today Show!
I was listening to the Van Morrison song, And the Healing Has Begun. The song resonates powerfully with Jean and me, in part because it was in our life together that the healing from our spouses’ deaths really began – and of course, thanks to David and John and Jeff and Janet and Susan and Sherry and others for keeping us pretty well until Jean and I met. Among the lines in that song that resonate most powerfully are:
We’re gonna stay out all night long
We’re gonna dance to the rock & roll
And then we’re gonna go out and roam across the field
The last time we stayed out all night long (other than at a hospital, LOL) was in 2018 when Jean and I were at a psytrance event thrown by the collective (Atrium Obscurum) that I’d been part of previously. It was a three-day, two-night party, but we were only there from Friday afternoon – Saturday morning. We worked the gate Friday evening (my last work with Atrium Obscurum) and hung with friends and then Ro’s Rage Against the Machine cover band played and then the opening ceremony and then the dancing began. We were awake through the night in our forest campsite, sharing words of love, kissing, making love while the music pulsed and people laughed and danced in the forest and over on the earth dance floor under the trees all through the night. In the morning we went to the dance floor, then to a yoga meeting with Kristina, and then we went swimming at the nearby spring-fed Lake Daingerfield. It was all magical…

At psytrance party
We’re gonna stay out all night long
We’re gonna dance to the rock & roll
And then we’re gonna go out and roam across the field
The music was psytrance instead of rock and roll and we swam in the cold spring waters instead of running across the field, but it’s all the same.
——————-
Searching through my blog for something related to Van singing And the Healing Has Begun I came across one loving post after another. Really a lot. Oh, the magic of our life together – where the healing really did begin! I’m awed by our reality then and now. I am so grateful to you, Jean. These days we sit naked in the warm waters of our hot tub with the moon shining, an owl hooting off to the north, and The City all lit up in the distance. What a time we’re having.
I found posts from 2017 and 2020 with the same title, Another Week in Berkeley. So here comes yet another week in Berkeley from now:
Tuesday, 2/13

Hot tub at sunset
We’re still chugging water to start the day, snack, meds, then our very own “Today Show” – what we see from our cosy, warm bed looking through the bedroom doors across San Francisco Bay, the Marin Headlands, Golden Gate Bridge, sky, clouds… talking, coffee, massage, ♥.
We’re still having fruit salad most days for breakfast: today it was pear, strawberries, blueberries, a little apple for the crunch, yogurt, maple syrup, toast, almond butter. After breakfast we had a soak in the hot tub (more on that in a moment).
Jean went to the dentist and I went to a Pilates session with Sandra. A few months ago Peter N-R gave me a session with her (Thanks, Peter!) and I’ve been going back weekly since then, except when I had covid.
We exchanged Valentine’s Day cards (more words of love). Jean and I fixed dinner: scallops in a simple, deep sauce with pasta and brocolinni.
Wednesday 2/14
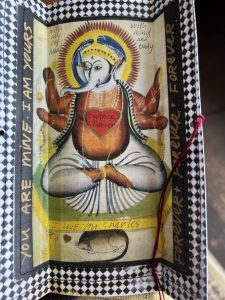
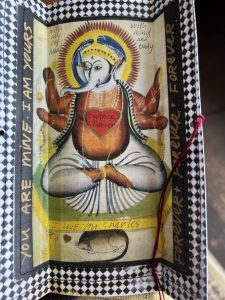
Jean made this Valentine’s Day card for me
Another day in Paradise, starting in the bed with meds, snack, mate, and the Today Show. First thing in the morning, hummingbirds fly straight up high in the air before they zip off to somewhere. There is a willow-related tree growing below our house and the top of the tree is eye-level for us. Hummingbirds like to perch on the very tip of the tip-top branches like little kings of their demesne.
Breakfast this morning was a “giant cookie”: oatmeal with strawberries and blueberries, Jean’s with butter and mine with almond butter, maple syrup, milk. As always, we ate together in the living room.
Afterward I drove to Solano Avenue, parked, and walked way down the street, then back up the other side, then to Peet’s, and then Andronico’s for strawberries, milk, and King Arthur flour.
After lunch we took a nap, then Jean went to Freida’s for haircut touch-up.
Exercise
I walked up to the Kensington market for ground beef and Jean fixed meat loaf, mashed potatoes, and broccolini for dinner, accompanied by Levain from Acme Bakery.
Since the pandemic began we’ve been watching television for an hour every night. Tonight we watched Sol Life on YouTube (the day-to-day solitary life of a woman in Japan) and part of a romantic comedy.

In the front garden
Thursday 2/15
Snack, water/electrolytes, meds, Peet’s for me and herbal tea for Jean, Today Show.
Hot tub, breakfast (kiwi from tree at Lisa’s studio, Asian pear, pear, strawberries, blueberries, banana, yogurt, toast and almond butter, granola).
I drove to the Berkeley Kaiser Permanente pharmacy to pick up Rx, then to nearby Berkeley Bowl for groceries. Home.
Lunch
Nap
Jean was in her studio in the late afternoon. I did Pilates exercise, went for a walk.
Jean fixed dinner – minestrone and I helped with prep and cleaned up.
Read
Friday 2/16
In the Today Show, huge fog banks covered most of the mountains/headlands so that it looked like big mountains in Colorado. We talked of the challenges we all face at this age, some of us more than others of us, some physical, some psychological/emotional, but all of us dealing with something significant.

Where we camped at psytrance party. Mid-left is the hard-to-see-in-the-day suspended heart that lit up the night.
We took a short hot tub.
Breakfast was (for Jean) smoked salmon on toast + fruit salad (Asian pear, pear, strawberries, blueberries, orange) and for me the same fruit salad with yogurt + toast and almond butter.
Jean went to the middle school pool for water walking with Janet and then a quick stop at Trader Joe’s. I walked up the street to the “top of the hill” and back down (~2,000 steps), then Pilates exercise.
Lunch was meat loaf, mashed potatoes, cheese, salsa sandwich for me and salad for Jean.
Nap, talking under the covers.
I made granola and Jean fixed a salad to go with the minestrone when Janet and Larry come over later.
Enjoyed judgment against Trump. I’m enjoying it very much!

A fence along where I walked
Had a nice Shabbat dinner (minestrone, salad, cheese with tangerines and chocolate for dessert) and fellowship with Jean’s oldest friend and her new partner, Larry. He says it’s a miracle to have this connection with Janet at this age. I concur – we’re all living a miracle!
Easy clean-up since most of the cooking done yesterday.
A TV show that once again showed that it’s a vast wasteland out there.
Sleep.
Saturday 2/17
Coffee, snack, meds, talk, Today Show, watching the sky transition from grey to pink to cloudy to clear, ♥. Hot tub.
Fruit salad, granola, yogurt.
Jean watching a podcast on Egyptian textiles and I’m writing this and reading more about Trump judgment. Got a text from Linda B: I’m going to sit for a portrait with her art group soon.
I’m problem solving re portable speaker and Jean is in her yoga room, then studio.
Lunch: another meat loaf sandwich for Mr. Adventures!

Stone wall, moss along where I walked
Nap together, lying in bed (again) talking.
I spent the rest of the afternoon writing, reading news feeds.
Jean was in the studio late afternoon, then came upstairs and fixed broiled salmon, salad, Acme levain.
Watched part of a French movie, L’Envol (Scarlet) – pretty good.
Slept.
Sunday 2/18
Coffee, snack, meds, talk, ♥. Hot tub.
Dishwasher not working, so we unloaded a full load and started washing dishes.
I fixed omelet with goat gouda cheese, mushrooms, green onions, levain, ½ sweet Italian sausage each for breakfast.
Washed dishes.
Talked with someone on the phone regarding how to prioritize and coordinate medical care with a spouse. Wrote f/u text.

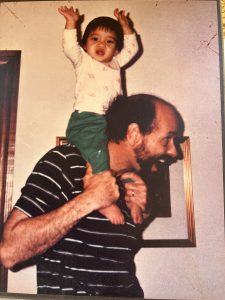
Jean in India about 10 years ago
Hi ——–,
In summary, the main problems that should be addressed quickly are:
Nausea and vomiting AND subsequent dehydration. There is an effective nausea medication (ondansetron) and he should have some at home as well as when in ER. There’s a good chance he’s dehydrated and in need of IV fluids now.
Pain – probably needing more than Tylenol or ibuprofen. Note that ibuprofen should be given with food to avoid stomach upset.
The past problem with ER should not influence you to avoid seeking care. They’ve already tried to make it right and may have to try more, but you should still go. You can also go to a different hospital. You should stick with him at ER to head off conflict.
The prostate and back are probably not priorities right now.
Wishing you and ——- well.
Charles
Went to MLK middle school track and we (or mostly Jean) walked with Susan. I’m using my iPhone to keep track of my steps these days. Most days I exceed my target.
Trader Joe for several things, including TJ salads for lunch
Lunch

Sunset from deck
Finish washing dishes
Nap, talking about life, including Jean’s friends M and V who recently died in their 90s, died within a few hours of one another, and lived independently and well in their house in the Berkeley Hills until death. There are many sad and even desperate stories happening among older people, including people we know. It’s well to remember M and V whose story is a triumph. And Jean’s friend, K, in her 90s, still in her home (with a fair amount of assistance). H and J, late 70s and early 80s, living in wooded hills near Point Reyes, growing quality cannabis. C and J, in their mid – late 70s, dealing with significant physical issues and living a beautiful life… We joined Ashby Village last year. Ashby Village is part of the village movement happening here and elsewhere. Through members and volunteers members work to remain in their homes as they age.
Talked with David.
Pilates exercise.
Writing this…

Fountain near the house
Reading news feeds. I read a lot of news. I think things are pretty horrible for many people around the world. I worry about the wars in Ukraine and Gaza. The news in the US, especially political news, is weird and unsettling. I’m unsettled.
Jean in studio.
Dinner was salmon in Indian curry paste (Sukhi’s brand) in coconut milk, cauliflower, slaw
Reading in living room, then taking a soak in the hot tub.
Watched movie, Scarlet) for an hour. Goodnight…
Monday 2/19
I woke up early and got up to write something re a neighborhood issue (whether the neighborhood forum is an appropriate place to discuss a petition to recall our county DA). Here’s what I wrote:
Reflecting on the question of politics entering this neighborhood discussion group, I see with greater clarity how much public safety and health are enmeshed in politics.
For me, personally, as I age and my physical abilities decline, a completely non-responsive Berkeley/Alamed a forces me to live with a cracked, uneven sidewalk in front of my house (only one fall, so far) and a shameful lack of bus benches for impaired AC Transit riders like me. Because of so much urine on downtown sidewalks, I had to spread newspapers on the sidewalk to sit when I was unable to stand while waiting for a bus. Like crime, these are public health/safety issues and any solution to them will include politics.
a forces me to live with a cracked, uneven sidewalk in front of my house (only one fall, so far) and a shameful lack of bus benches for impaired AC Transit riders like me. Because of so much urine on downtown sidewalks, I had to spread newspapers on the sidewalk to sit when I was unable to stand while waiting for a bus. Like crime, these are public health/safety issues and any solution to them will include politics.
I appreciate the opportunity to step out of my kitchen door to sign a petition to recall. I felt no pressure to sign. And I don’t feel there is a risk to neighborhood cohesion or relationships related to this discussion!
Fixed coffee, snack, meds, lay in bed talking, ♥.
Oh! There’s a rainbow over The Bay!
Hot tub
Fruit for breakfast: Asian pear, pear, grapes, blueberries, strawberries, apple
Worked on medications
Installed color toner cartridges in color laser printer. I am smrt! I am smrt!

Night sky
Lunch: granola for me, smoked salmon and goat cheese for Jean.
Nap
I did a lot of nothing from 3-5:30, then to Sol’s for dinner. Sabich sandwich for me, mesquite smoked trout for Jean. Best trout since I lived in Colorado. Jean agreed.
Hot tub.
I chose the evening’s entertainment: Seinfeld and Young Sheldon.
It rained during the night.
That’s another week in Berkeley.
About the hot tub: I gave Jean a hot tub (or spa) for Christmas and she paid for retrofitting the deck so we could have the tub on the same level as bedroom and living room. It’s exactly 20 steps from the tub to the shower. Nice! Thank you, Sweet Thing!

Highway from Marathon to Big Bend. We’ll be on that road in a few weeks on our trip to Marfa and Big Bend
 I found the first explication of what I was trying to trying to do for most of my life. It is in a memorandum written in 1978 to Elsie Griffith, the executive director of the Dallas Visiting Nurse Association. At the time, I was working on planning and implementing the VNA Terminal Care Program, which was foundational for the first hospice in Texas. In hospice we focused intensively on managing physical symptoms at the end-of-life, such as pain, nausea, shortness of breath, etc.; and on supporting families. The subject here is the spiritual and ethical structuring of this work. It’s hard to believe I sent this and that Elsie accepted it and believed in the vision. Here it is, exactly as I sent it:
I found the first explication of what I was trying to trying to do for most of my life. It is in a memorandum written in 1978 to Elsie Griffith, the executive director of the Dallas Visiting Nurse Association. At the time, I was working on planning and implementing the VNA Terminal Care Program, which was foundational for the first hospice in Texas. In hospice we focused intensively on managing physical symptoms at the end-of-life, such as pain, nausea, shortness of breath, etc.; and on supporting families. The subject here is the spiritual and ethical structuring of this work. It’s hard to believe I sent this and that Elsie accepted it and believed in the vision. Here it is, exactly as I sent it: